Modulation by Docosahexaenoic Acid of a Novel Potential Biomarker of Cognitive Decline
This article at a glance
- Prevention of Alzheimer’s disease by intervention at earlier stages of cognitive decline is increasingly viewed as an alternative approach to the not yet achieved successful treatment of Alzheimer’s disease.
- This exploratoy study makes a preliminary evaluation of neuronal pentraxin 1 (NP1) as a new biomarker of cognitive decline, that reflects synaptic loss.
- Increased plasma NP1 levels were detected in patients with mild cognitive impairment and early Alzheimer’s disease.
- The biomarker is sensitive to the intake of docosahexaenoic acid (DHA) in a mouse for Alzheimer’s disease, supporting further attention to the need for adequacy in omega-3 long chain polyunsaturated fatty acid levels in Alzheimer’s disease prevention.
The prevalence of Alzheimer’s disease keeps increasing as the elderly population of many countries in the Western world is growing. While much effort has been made in developing treatments for this neurodegenerative disease, there is still no cure, and the progressive loss of cognitive abilities can, at best, be delayed. The signs and symptoms of Alzheimer’s disease are relatively well documented, but an effective treatment is still a large and unmet goal. Since major progress for effective pharmacotherapy currently appears to be out of reach, increased focus is being placed on prevention or addressing the disorder at earlier stages of cognitive decline, that precede the diagnosis of Alzheimer’s disease. The identification of individuals at risk of Alzheimer's disease, but who do not yet show evidence of neurodegeneration is now considered to be crucial to the success of any preventive approaches.
The characteristic changes in this disease are the formation of specific protein deposits in brain tissue, namely of extracellular diffuse plaques of aggregated amyloid beta (Aβ) peptide, and intracellular tangles of hyper-phosphorylated tau protein. There is evidence that the formation of Aβ peptide aggregates occurs initially within the neuronal cell bodies and is involved in the loss of neuronal interactions and synaptic plasticity. Carrying the apolipoprotein E4 (ApoE4) allele is the main risk factor for late-onset Alzheimer’s disease, and different apoE forms modulate disease susceptibility. Apolipoprotein E directly interacts with Aβ aggregates, with ApoE4 displaying higher binding than other apolipoprotein isoforms, such as ApoE2 and ApoE3. Microglial cells in brain tissue mount innate immune responses to amyloid peptide aggregates, and these reactions also involve apolipoprotein E, thereby further propagating brain tissue-damaging reactions.
The development of pharmacological approaches that reduce Aβ aggregate formation, or which promote Aβ deposit removal from brain tissue has been achieved, but has to date not been translated into a marked clinical benefit for Alzheimer’s disease patients. This is possibly because at the stage when Aβ plaques are already present, the disease has progressed to a point where irreversible neurodegeneration has already occurred. Research into improving pharmacotherapy is nevertheless still advancing, with promising combinatorial approaches that target the production of Aβ and promote the clearance of Aβ plaques from the brain. A more pessimistic view is that targeting Aβ will not be successful because it does little in modifying the more fundamental, although still largely unclear, primary causes of Alzheimer’s disease.
An alternative approach that has been gaining more attention recently is the intervention prior to the transition of mild cognitive decline into the early stages of Alzheimer’s disease. To that end, it is necessary to know which markers are selective enough to detect the earliest stages of neurodegeneration and cognitive decline, have sufficient predictive value for the future development of Alzheimer’s disease, and are sensitive enough to determine the effect of testable interventions at such early stages for long-term prevention interventions to work. A recently developed test for early detection compares the ratio of pathological and normal forms of Aβ in blood. The test can detect pathogenic Aβ not only in those patients already exhibiting early symptoms of Alzheimer’s disease, but also already 8 years in advance of symptom development. Ideally, lifestyle modifications and/or pharmacological interventions should be commenced when early signs prior to transitioning into Alzheimer’s disease would be detected.
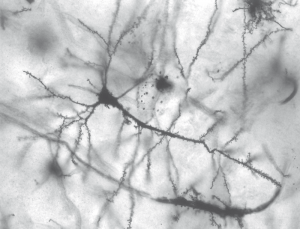
A recent study has investigated the suitability of a different biomarker for early detection of risk of developing Alzheimer’s disease. Instead of focusing on the hallmark Aβ peptide, the researchers evaluated the possibility to detect early signs of synaptic loss occurring within the brain, in a way that would be measurable in blood. The study was performed by Ma and colleagues from the Department of Neurology, at the David Geffen School of Medicine, University of California, several other institutions in the U.S.A and the Department of Neurology at Sun Yat-sen University, Guangzhou, China. The researchers examined the relationship of the protein neuronal pentraxin 1 (NP1) with cognitive decline. NP1 is secreted from excitatory neurons in the central nervous system and regulates various aspects of synapse formation and neuronal excitability. Importantly, increased NP1 levels have also been associated with neurodegeneration and Alzheimer plaque pathology. To assess the potential value of NP1 as a biomarker for synapse loss in the central nervous system, studies were carried out in a mouse model of Alzheimer’s disease, and in people with mild cognitive decline known to be at risk of transitioning to Alzheimer’s disease.
First, the researchers used mice that carried one allele of apolipoprotein ɛ4 (ApoE4+/-) and/or the transgenic expression of mutations in five genes involved in a condition known as Familial Alzheimer’s Disease (FAD). In this murine Alzheimer’s disease model, mutations in several amyloid beta-processing enzymes drive rapid Aβ-42 peptide generation in an additive manner, with the mice developing cerebral amyloid plaques at 2 months of age, and displaying reduced synaptic markers, neuron loss, and memory impairment. These “E4FAD” mice had markedly increased levels of NP1 in plasma, compared to E3FAD mice carrying two apolipoprotein E3 alleles (Apo3+/+). These mice had also received a diet between 3 and 7 months containing 5% fat and a relatively high level of linoleic acid. Interestingly, when 0.6% docosahexaenoic acid (DHA)-rich oil was also included in the diet, NP1 levels in the E4FAD were restored to the same level as in the E3FAD mice. Mice that did not contain the FAD mutations (E4FAD– mice) also displayed a lower level of NP1 in plasma than the E4FAD mice.
The NP1 level in the hippocampus was also increased in E4FAD mice but normalized by consumption of the DHA-enriched diet. Lower expression of NP1 in the hippocampus of E4FAD- mice was confirmed by immunohistochemical analysis. Furthermore, when Aβ42 oligomers were directly infused into the brain of normal mice, the formation of Aβ aggregates was observed in the dentate gyrus of the hippocampus. In this model of Alzheimer’s disease, NP1 expression was increased in the same brain area, suggesting that its expression follows amyloid plaque formation and associated hippocampal neuronal injury. The research also identified NP1 in exosomes, small micron-sized membrane vesicles that are released from cells, which could reflect a way whereby brain NP1 is transported into the systemic circulation. In summary, these exploratory studies show that NP1 levels in mice are determined by the genotype for the apolipoprotein E and FAD genes that are important risk factors for Alzheimer’s disease in humans. Interestingly, this synaptic function biomarker may be sensitive to DHA intake via the diet.
To evaluate if NP1 might have any potential predictive value for synaptic loss and neurodegeneration in humans, the researchers examined plasma samples from the ImaGene Study (Imaging and Genetic Biomarkers for Alzheimer Disease), a longitudinal cohort study of people over 50 years old with mild cognitive decline. Individuals with mild cognitive decline had significantly increased plasma levels of NP1 compared to matched individuals with normal cognitive ability. In people with early stage Alzheimer’s Disease, plasma NP1 levels were further elevated. There was a trend (P=0.078) towards higher plasma NP1 levels in ApoE4 carriers compared with ApoE4-negative individuals.
The results of this study suggest that NP-1 is an interesting new biomarker that could potentially be explored further for its value in detecting early cognitive decline that is associated with specific biochemical changes related to reductions in neuronal signaling in the brain. Furthermore, the results suggest that this functional biomarker may be sensitive to modulation by increased DHA intake. Of note, the apolipoprotein E4 genotype is associated with abnormal handling of DHA by the body. Studies have shown that APOE4 carriers do not increase tissue status of omega-3 LCPUFA following EPA/DHA dietary supplementation as well as non-carriers.
The results of this study are interesting but need to be viewed as exploratory and instructive for future research. Validation of a biomarker for cognitive function is hard but could be well worth the effort if it allows physicians to detect cognitive decline many years ahead of Alzheimer’s disease. Knowing that this biomarker is sensitive to dietary modulation provides an additional incentive to work towards this goal.
Ma QL, Teng E, Zuo X, Jones M, Teter B, Zhao EY, Zhu C, Bilousova T, Gylys KH, Apostolova LG, LaDu MJ, Hossain MA, Frautschy SA, Cole GM. Neuronal pentraxin 1: A synaptic-derived plasma biomarker in Alzheimer's disease. Neurobiol. Dis. 2018;114:120-128. [PubMed]
Worth Noting
Abad MA, Enguita M, DeGregorio-Rocasolano N, Ferrer I, Trullas R. Neuronal pentraxin 1 contributes to the neuronal damage evoked by amyloid-beta and is overexpressed in dystrophic neurites in Alzheimer's brain. J. Neurosci. 2006;26(49):12735-12747. [PubMed]
Carter DB. The interaction of amyloid-beta with ApoE. Subcell. Biochem. 2005;38:255-272. [PubMed]
Chouinard-Watkins R, Conway V, Minihane AM, Jackson KG, Lovegrove JA, Plourde M. Interaction between BMI and APOE genotype is associated with changes in the plasma long-chain-PUFA response to a fish-oil supplement in healthy participants. Am. J. Clin. Nutr. 2015;102(2):505-513. [PubMed]
Farhy-Tselnicker I, van Casteren ACM, Lee A, Chang VT, Aricescu A, Allen NJ. Astrocyte-secreted glypican 4 regulates release of neuronal pentraxin 1 from axons to induce functional synapse formation. Neuron. 2017;96(2):428-445. [PubMed]
Figueiro-Silva J, Gruart A, Clayton KB, Podlesniy P, Abad MA, Gasull X, Delgado-García JM, Trullas R. Neuronal pentraxin 1 negatively regulates excitatory synapse density and synaptic plasticity. J. Neurosci. 2015;35(14):5504-5521. [PubMed]
ImaGene Study - Imaging and Genetic Biomarkers for Alzheimer Disease Study, Mary S. Easton center for Alzheimer’s Disease Research Center at UCLA.
Lee SJ, Wei M, Zhang C, Maxeiner S, Pak C, Calado Botelho S, Trotter J, Sterky FH, Südhof TC. Presynaptic neuronal pentraxin receptor organizes excitatory and inhibitory synapses. J. Neurosci. 2017;37(5):1062-1080. [PubMed]
Meredith SC. Protein denaturation and aggregation: Cellular responses to denatured and aggregated proteins. Ann. N Y Acad. Sci. 2005;1066:181-221. [PubMed]
Nabers A, Perna L, Lange J, Mons U, Schartner J, Güldenhaupt J, Saum KU, Janelidze S, Holleczek B, Rujescu D, Hansson O, Gerwert K, Brenner H. Amyloid blood biomarker detects Alzheimer's disease. EMBO Mol. Med. 2018;Apr 6:e8763. [PubMed]
Oakley H, Cole SL, Logan S, Maus E, Shao P, Craft J, Guillozet-Bongaarts A, Ohno M, Disterhoft J, Van Eldik L, Berry R, Vassar R. Intraneuronal beta-amyloid aggregates, neurodegeneration, and neuron loss in transgenic mice with five familial Alzheimer's disease mutations: potential factors in amyloid plaque formation. J. Neurosci. 2006;26(40):10129-10140. [PubMed]
Patel TK, Holtzman DM. Dual therapy for Aβ amyloidosis in AD: A successful one-two combo. J. Exp. Med. 2018;April 23. [Link]
Ulrich JD, Ulland TK, Mahan TE, Nyström S, Nilsson KP, Song WM, Zhou Y, Reinartz M, Choi S, Jiang H, Stewart FR, Anderson E, Wang Y, Colonna M, Holtzman DM. ApoE facilitates the microglial response to amyloid plaque pathology. J. Exp. Med. 2018;215(4):1047. [PubMed]
Yassine HN. Targeting prodromal Alzheimer's disease: too late for prevention? Lancet Neurol. 2017;16(12):946-947. [PubMed]

