Heart Health Benefits of EPA and DHA
GOED/Omega-3 Science Advisory Council
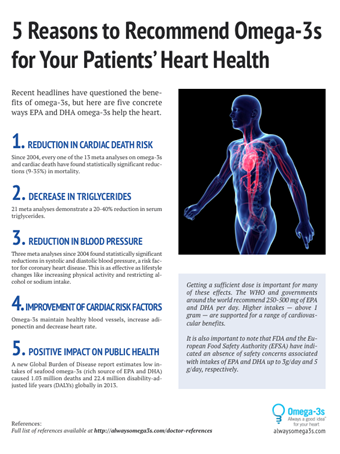
White Paper Decades of research have uncovered many health benefits of long-chain omega-3 fatty acids, specifically eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). EPA and DHA are both essential building blocks for tissue structures and important biological mediators in health and disease, which is why the Dietary Guidelines for Americans, as well as health advocacy groups from around the globe, recommend eating foods rich in EPA and DHA as part of an overall healthy eating pattern. Yet, there are mixed viewpoints about the cardiovascular benefits of EPA and DHA when taken in supplement form. This document reviews the scientific evidence about EPA and DHA and its association with cardiovascular health and disease risk reduction.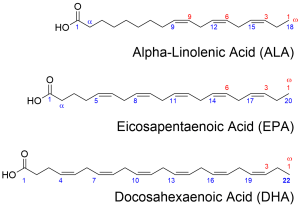 Omega-3 Basics There are three primary omega-3 fatty acids consumed in the diet: alpha linolenic acid (ALA), EPA and DHA. All are polyunsaturated fatty acids with varying lengths of the carbon backbone. ALA has 18 carbon atoms with three double bonds; EPA has 20 carbon atoms and five double bonds; and DHA has 22 carbon atoms and six double bonds. ALA is found in plant foods such as soybeans, black walnuts, flaxseeds, and chia, whereas EPA and DHA are marine-based and found in seafood (especially fatty fish). Sources of EPA and DHA for supplements include sardines, anchovies, certain types of algae and krill. While the body can elongate ALA into its longer-chain omega-3 fatty acid counterparts, the process is inefficient with less than 5 percent converting to EPA and less than 1 percent to DHA. The best way to get EPA and DHA is by consuming it directly, through foods and supplements. Why EPA and DHA are Important The roles and functions of EPA and DHA are distinct but complementary. As precursors to several families of biologically active molecules (resolvins, protectins, maresins, prostaglandins, leukotrienes, etc.), EPA and DHA both help to control inflammatory responses and regulate blood coagulation. They both play a role in determining what genes are turned on and off. DHA, by virtue of its greater presence in cell membranes than EPA, plays an important structural role in cells, helping make cell walls more flexible. This in turn allows the proteins in the membrane to control the inflow and outflow of important cell components, making the cell operate most efficiently. DHA is found in virtually all cells, but it is particularly concentrated in cells of the brain, heart and retina. EPA and DHA and Heart Health What Is Known Scores of research studies support the view that EPA and DHA omega-3s are cardioprotective nutrients. Higher intakes or blood levels of these important fatty acids are associated with reduced risk of mortality from coronary heart disease (CHD) and sudden cardiac death.1 The USDA’s National Evidence Library notes that the evidence supporting EPA and DHA for heart health is “moderate” indicating that some of the evidence is conflicting and more research needs to be done.1 Importantly, recent meta-analyses of randomized-controlled studies found that dosages greater than 1 gram (1,000 mg) EPA+DHA per day offer significant cardioprotection,2 reducing risk for CHD by 20 percent or greater.3 Studies with even lower intakes find that overall risk for cardiac death is reduced,4 and a recent modeling exercise looking at prospective studies found that intake of EPA+DHA at any dose level was associated with reduced risk for any type of CHD event.5 EPA and DHA, especially at relatively high doses (i.e. >3 g/day), have been shown to lower triglycerides and raise HDL-cholesterol (the “good” cholesterol).6 The same study found that in patients with extremely elevated triglyceride levels, fish oil supplementation may also slightly raise LDL-cholesterol, yet total cholesterol remained virtually unchanged. Other studies have also found that EPA+DHA improve blood vessel function,7 reduce inflammation,8 and lower blood pressure.9 What is Unclear and Needs More Research Several major early studies using fish or fish oils to reduce CHD events were favorable. These included DART,10 JELIS,11 and two GISSI12,13 studies. It was upon the basis of two studies (DART and GISSI-Prevenzione) that most recommendations in the late 1990s and early 2000s for the use of EPA+DHA in secondary prevention were founded. However, at least six trials published between 2010 and 2014 did not find a benefit for EPA+DHA in patients with known CHD or with risk factors for heart disease.14-19 These “failed” studies obviously beg the question of whether, in today’s world of modern medical care, omega-3 fatty acid supplementation still reduces risk for CHD. It’s a reasonable question, because even though the safety of EPA and DHA supplementation is certain, consumers – and their healthcare providers – may express concern about the cost and/or inconvenience of supplementation when the perceived benefits are not as clear. These are valid concerns. But before any conclusions can be drawn about fish oils and EPA/DHA supplements failing to prevent heart disease, we need to interpret findings of recent clinical studies in context. That is to say that if we are going to accept the findings of these studies, then we must keep in mind the conditions under which they were done. When we do so, we find that fish oils “did not work” in the following setting where patients:
Omega-3 Basics There are three primary omega-3 fatty acids consumed in the diet: alpha linolenic acid (ALA), EPA and DHA. All are polyunsaturated fatty acids with varying lengths of the carbon backbone. ALA has 18 carbon atoms with three double bonds; EPA has 20 carbon atoms and five double bonds; and DHA has 22 carbon atoms and six double bonds. ALA is found in plant foods such as soybeans, black walnuts, flaxseeds, and chia, whereas EPA and DHA are marine-based and found in seafood (especially fatty fish). Sources of EPA and DHA for supplements include sardines, anchovies, certain types of algae and krill. While the body can elongate ALA into its longer-chain omega-3 fatty acid counterparts, the process is inefficient with less than 5 percent converting to EPA and less than 1 percent to DHA. The best way to get EPA and DHA is by consuming it directly, through foods and supplements. Why EPA and DHA are Important The roles and functions of EPA and DHA are distinct but complementary. As precursors to several families of biologically active molecules (resolvins, protectins, maresins, prostaglandins, leukotrienes, etc.), EPA and DHA both help to control inflammatory responses and regulate blood coagulation. They both play a role in determining what genes are turned on and off. DHA, by virtue of its greater presence in cell membranes than EPA, plays an important structural role in cells, helping make cell walls more flexible. This in turn allows the proteins in the membrane to control the inflow and outflow of important cell components, making the cell operate most efficiently. DHA is found in virtually all cells, but it is particularly concentrated in cells of the brain, heart and retina. EPA and DHA and Heart Health What Is Known Scores of research studies support the view that EPA and DHA omega-3s are cardioprotective nutrients. Higher intakes or blood levels of these important fatty acids are associated with reduced risk of mortality from coronary heart disease (CHD) and sudden cardiac death.1 The USDA’s National Evidence Library notes that the evidence supporting EPA and DHA for heart health is “moderate” indicating that some of the evidence is conflicting and more research needs to be done.1 Importantly, recent meta-analyses of randomized-controlled studies found that dosages greater than 1 gram (1,000 mg) EPA+DHA per day offer significant cardioprotection,2 reducing risk for CHD by 20 percent or greater.3 Studies with even lower intakes find that overall risk for cardiac death is reduced,4 and a recent modeling exercise looking at prospective studies found that intake of EPA+DHA at any dose level was associated with reduced risk for any type of CHD event.5 EPA and DHA, especially at relatively high doses (i.e. >3 g/day), have been shown to lower triglycerides and raise HDL-cholesterol (the “good” cholesterol).6 The same study found that in patients with extremely elevated triglyceride levels, fish oil supplementation may also slightly raise LDL-cholesterol, yet total cholesterol remained virtually unchanged. Other studies have also found that EPA+DHA improve blood vessel function,7 reduce inflammation,8 and lower blood pressure.9 What is Unclear and Needs More Research Several major early studies using fish or fish oils to reduce CHD events were favorable. These included DART,10 JELIS,11 and two GISSI12,13 studies. It was upon the basis of two studies (DART and GISSI-Prevenzione) that most recommendations in the late 1990s and early 2000s for the use of EPA+DHA in secondary prevention were founded. However, at least six trials published between 2010 and 2014 did not find a benefit for EPA+DHA in patients with known CHD or with risk factors for heart disease.14-19 These “failed” studies obviously beg the question of whether, in today’s world of modern medical care, omega-3 fatty acid supplementation still reduces risk for CHD. It’s a reasonable question, because even though the safety of EPA and DHA supplementation is certain, consumers – and their healthcare providers – may express concern about the cost and/or inconvenience of supplementation when the perceived benefits are not as clear. These are valid concerns. But before any conclusions can be drawn about fish oils and EPA/DHA supplements failing to prevent heart disease, we need to interpret findings of recent clinical studies in context. That is to say that if we are going to accept the findings of these studies, then we must keep in mind the conditions under which they were done. When we do so, we find that fish oils “did not work” in the following setting where patients: - were given a < 1 g/day for about 2-3 years (i.e., a low dose for a short period of time);
- were in their early 60s;
- were typically on one to five other heart/diabetes medicines and had been treated in the hospital immediately after their heart attack to restore blood flow to the heart muscle (which greatly reduces the damage); and
- whose background omega-3 intake (from diet) was close to a cardioprotective dose already (i.e., around 250 mg/d).
- In addition, most of these studies included too few of the specific kinds of heart attacks most likely to benefit from omega-3 to draw any valid statistical conclusions. These concerns have been raised by several experts in the field.20-24 Under these conditions, it is not surprising at all that the addition of a relatively small amount of EPA and DHA had no detectable effect.
 The flyer is designed to be distributed to patients and colleagues and can be found here (https://drive.google.com/file/d/0B6uJWj5y9FY9NzJMV2xvbmlqWEk/view?usp=sharing). References: 1. U.S. Department of Agriculture Nutrition Evidence Library. “What is the relationship between consumption of seafood n-3 fatty acids and the risk of cardiovascular disease?” Accessed October 29, 2015. http://www.nel.gov/evidence.cfm?evidence_summary_id=250321. 2. Wen YT, Dai JH, Gao Q. Effects of Omega-3 fatty acid on major cardiovascular events and mortality in patients with coronary heart disease: a meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. 2014;24:470-5. [PubMed] 3. Casula M, Soranna D, Catapano AL, Corrao G. Long-term effect of high dose omega-3 fatty acid supplementation for secondary prevention of cardiovascular outcomes: A meta-analysis of randomized, double blind, placebo controlled trials. Atheroscler Suppl. 2013;14:243-51. [PubMed] 4. Trikalinos TA, Lee J, Moorthy D, Yu WW, Lau J, Lichtenstein AH, Chung M. Effects of Eicosapentanoic Acid and Docosahexanoic Acid on Mortality Across Diverse Settings: Systematic Review and Meta-analysis of Randomized Trials and Prospective Cohorts. Technical Review 17, Vol. 4. (Prepared by the Tufts Medical Center Evidence-based Practice Center under Contract No. HHSA 290-2007-10055-1.) AHRQ Publication No. 12-EHC040-EF. Rockville, MD: Agency for Healthcare Research and Quality; February 2012. [PubMed] 5. Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, et al. Association of Dietary, Circulating, and Supplement Fatty Acids With Coronary Risk: A Systematic Review and Meta-analysis. Ann Intern Med. 2014; 160:398-406. [PubMed] 6. Eslick GD, Howe PR, Smith C, Priest R, Bensoussan A. Benefits of fish oil supplementation in hyperlipidemia: a systematic review and meta-analysis. Int J Cardiol. 2009;136:4-16. [PubMed] 7. Nestel P, Shige H, Pomeroy S, Cehun M, Abbey M, Raederstorff D. The n-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid increase systemic arterial compliance in humans. Am J Clin Nutr. 2002;76:326-30. [PubMed] 8. Li K, Huang T, Zheng J, Wu K, Li D. Effect of marine-derived n-3 polyunsaturated fatty acids on C-reactive protein, interleukin 6 and tumor necrosis factor alpha: a meta-analysis. PLoS One. 2014;9:e88103. [PubMed] 9. Miller PE, Van Elswyk M, Alexander DD. Long-chain omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid and blood pressure: a meta-analysis of randomized controlled trials. Am J Hyperten. 2014;27:885-96. [PubMed] 10. Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989;2:757-61. [PubMed] 11. Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369:1090-8. [PubMed] 12. Marchioli R, Barzi F, Bomba E, Chieffo C, Di Gregorio D, Di Mascio R, et al. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI)-Prevenzione. Circulation. 2002;105:1897-903. [PubMed] 13. Investigators GISSI-Heart Failure Study. Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:1223-30. [PubMed] 14. Rauch B, Schiele R, Schneider S, Diller F, Victor N, Gohlke H, et al. OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Circulation. 2010;122:2152-9. [PubMed] 15. Bosch J, Gerstein HC, Dagenais GR, Diaz R, Dyal L, Jung H, et al. n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med. 2012;367:309-18. [PubMed] 16. Bonds DE, Harrington M, Worrall BB, Bertoni AG, Eaton CB, Hsia J, et al. Effect of long-chain omega-3 fatty acids and lutein + zeaxanthin supplements on cardiovascular outcomes: results of the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA Intern Med. 2014;174:763-71. [PubMed] 17. Galan P, Kesse-Guyot E, Czernichow S, Briancon S, Blacher J, Hercberg S. Effects of B vitamins and omega 3 fatty acids on cardiovascular diseases: a randomised placebo controlled trial. BMJ. 2010;341:c6273. [PubMed] 18. Roncaglioni MC, Tombesi M, Avanzini F, Barlera S, Caimi V, Longoni P, et al. n-3 fatty acids in patients with multiple cardiovascular risk factors. N Engl J Med. 2013;368:1800-8. [PubMed] 19. Kromhout D, Giltay EJ, Geleijnse JM. n-3 fatty acids and cardiovascular events after myocardial infarction. NEnglJ Med. 2010;363:2015-26. [PubMed] 20. Harris WS. Are n-3 fatty acids still cardioprotective? Curr Opin Clin Nutr Metab Care. 2013;16:141-9. [PubMed] 21. James MJ, Sullivan TR, Metcalf RG, Cleland LG. Pitfalls in the use of randomised controlled trials for fish oil studies with cardiac patients. Br J Nutr. 2014;112:812-20. [PubMed] 22. von Schacky C. Omega-3 fatty acids in cardiovascular disease--an uphill battle. Prostaglandins Leukot Essent Fatty Acids. 2015;92:41-7. [PubMed] 23. Marchioli R, Levantesi G. n-3 PUFAs in cardiovascular disease. Int J Cardiol. 2013;170:S33-8. [PubMed] 24. Wu JH, Mozaffarian D. Omega-3 fatty acids, atherosclerosis progression and cardiovascular outcomes in recent trials: new pieces in a complex puzzle. Heart. 2014;100:530-3. [PubMed] 25. US Department of Health and Human Services, Food and Drug Administration. 21 CFR part 184 [docket no. 86G-0289]. June 5, 1997. [Link] 26. Wachira JK, Larson MK, Harris WS. n-3 Fatty acids affect haemostasis but do not increase the risk of bleeding: clinical observations and mechanistic insights. Br J Nutr. 2014;111:1652-62. [PubMed] 27. U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: U.S. Government Printing Office, December 2010. [Link] 28. Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82-96. [PubMed] 29. Fatty Acids in Human Nutrition: Report of an expert consultation. FAO Food and Nutrition Paper, 91. November 10-14, 2008. http://www.fao.org/fileadmin/user_upload/nutrition/docs/requirements/fatsandfattacidsreport.pdf 30. International Society for the Study of Fatty Acids and Lipids (ISSFAL) Report on Dietary Intake of Essential Fatty Acids. Recommendations for Dietary Intake of Polyunsaturated Fatty Acids in Healthy Adults, June 2004. [Link] 31. Vannice G, Rasmussen H. Position of the Academy of Nutrition and Dietetics: dietary fatty acids for healthy adults. J Acad Nutr Diet. 2014;114:136-53. [PubMed] 32. Papanikolaou Y, Brooks J, Reider C and Fulgoni VL 3rd. U.S. adults are not meeting recommended levels for fish and omega-3 fatty acid intake: results of an analysis using observational data from NHANES 2003–2008. Nutr J. 2014;13:31. [PubMed] This Invited Opinion paper was written and prepared by the Global Organization for EPA and DHA (GOED), in collaboration with the Omega-3 Science Advisory Council (http://alwaysomega3s.com/see/science-advisory-council) Corresponding author:
The flyer is designed to be distributed to patients and colleagues and can be found here (https://drive.google.com/file/d/0B6uJWj5y9FY9NzJMV2xvbmlqWEk/view?usp=sharing). References: 1. U.S. Department of Agriculture Nutrition Evidence Library. “What is the relationship between consumption of seafood n-3 fatty acids and the risk of cardiovascular disease?” Accessed October 29, 2015. http://www.nel.gov/evidence.cfm?evidence_summary_id=250321. 2. Wen YT, Dai JH, Gao Q. Effects of Omega-3 fatty acid on major cardiovascular events and mortality in patients with coronary heart disease: a meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. 2014;24:470-5. [PubMed] 3. Casula M, Soranna D, Catapano AL, Corrao G. Long-term effect of high dose omega-3 fatty acid supplementation for secondary prevention of cardiovascular outcomes: A meta-analysis of randomized, double blind, placebo controlled trials. Atheroscler Suppl. 2013;14:243-51. [PubMed] 4. Trikalinos TA, Lee J, Moorthy D, Yu WW, Lau J, Lichtenstein AH, Chung M. Effects of Eicosapentanoic Acid and Docosahexanoic Acid on Mortality Across Diverse Settings: Systematic Review and Meta-analysis of Randomized Trials and Prospective Cohorts. Technical Review 17, Vol. 4. (Prepared by the Tufts Medical Center Evidence-based Practice Center under Contract No. HHSA 290-2007-10055-1.) AHRQ Publication No. 12-EHC040-EF. Rockville, MD: Agency for Healthcare Research and Quality; February 2012. [PubMed] 5. Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, et al. Association of Dietary, Circulating, and Supplement Fatty Acids With Coronary Risk: A Systematic Review and Meta-analysis. Ann Intern Med. 2014; 160:398-406. [PubMed] 6. Eslick GD, Howe PR, Smith C, Priest R, Bensoussan A. Benefits of fish oil supplementation in hyperlipidemia: a systematic review and meta-analysis. Int J Cardiol. 2009;136:4-16. [PubMed] 7. Nestel P, Shige H, Pomeroy S, Cehun M, Abbey M, Raederstorff D. The n-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid increase systemic arterial compliance in humans. Am J Clin Nutr. 2002;76:326-30. [PubMed] 8. Li K, Huang T, Zheng J, Wu K, Li D. Effect of marine-derived n-3 polyunsaturated fatty acids on C-reactive protein, interleukin 6 and tumor necrosis factor alpha: a meta-analysis. PLoS One. 2014;9:e88103. [PubMed] 9. Miller PE, Van Elswyk M, Alexander DD. Long-chain omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid and blood pressure: a meta-analysis of randomized controlled trials. Am J Hyperten. 2014;27:885-96. [PubMed] 10. Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989;2:757-61. [PubMed] 11. Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369:1090-8. [PubMed] 12. Marchioli R, Barzi F, Bomba E, Chieffo C, Di Gregorio D, Di Mascio R, et al. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI)-Prevenzione. Circulation. 2002;105:1897-903. [PubMed] 13. Investigators GISSI-Heart Failure Study. Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:1223-30. [PubMed] 14. Rauch B, Schiele R, Schneider S, Diller F, Victor N, Gohlke H, et al. OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Circulation. 2010;122:2152-9. [PubMed] 15. Bosch J, Gerstein HC, Dagenais GR, Diaz R, Dyal L, Jung H, et al. n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med. 2012;367:309-18. [PubMed] 16. Bonds DE, Harrington M, Worrall BB, Bertoni AG, Eaton CB, Hsia J, et al. Effect of long-chain omega-3 fatty acids and lutein + zeaxanthin supplements on cardiovascular outcomes: results of the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA Intern Med. 2014;174:763-71. [PubMed] 17. Galan P, Kesse-Guyot E, Czernichow S, Briancon S, Blacher J, Hercberg S. Effects of B vitamins and omega 3 fatty acids on cardiovascular diseases: a randomised placebo controlled trial. BMJ. 2010;341:c6273. [PubMed] 18. Roncaglioni MC, Tombesi M, Avanzini F, Barlera S, Caimi V, Longoni P, et al. n-3 fatty acids in patients with multiple cardiovascular risk factors. N Engl J Med. 2013;368:1800-8. [PubMed] 19. Kromhout D, Giltay EJ, Geleijnse JM. n-3 fatty acids and cardiovascular events after myocardial infarction. NEnglJ Med. 2010;363:2015-26. [PubMed] 20. Harris WS. Are n-3 fatty acids still cardioprotective? Curr Opin Clin Nutr Metab Care. 2013;16:141-9. [PubMed] 21. James MJ, Sullivan TR, Metcalf RG, Cleland LG. Pitfalls in the use of randomised controlled trials for fish oil studies with cardiac patients. Br J Nutr. 2014;112:812-20. [PubMed] 22. von Schacky C. Omega-3 fatty acids in cardiovascular disease--an uphill battle. Prostaglandins Leukot Essent Fatty Acids. 2015;92:41-7. [PubMed] 23. Marchioli R, Levantesi G. n-3 PUFAs in cardiovascular disease. Int J Cardiol. 2013;170:S33-8. [PubMed] 24. Wu JH, Mozaffarian D. Omega-3 fatty acids, atherosclerosis progression and cardiovascular outcomes in recent trials: new pieces in a complex puzzle. Heart. 2014;100:530-3. [PubMed] 25. US Department of Health and Human Services, Food and Drug Administration. 21 CFR part 184 [docket no. 86G-0289]. June 5, 1997. [Link] 26. Wachira JK, Larson MK, Harris WS. n-3 Fatty acids affect haemostasis but do not increase the risk of bleeding: clinical observations and mechanistic insights. Br J Nutr. 2014;111:1652-62. [PubMed] 27. U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: U.S. Government Printing Office, December 2010. [Link] 28. Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82-96. [PubMed] 29. Fatty Acids in Human Nutrition: Report of an expert consultation. FAO Food and Nutrition Paper, 91. November 10-14, 2008. http://www.fao.org/fileadmin/user_upload/nutrition/docs/requirements/fatsandfattacidsreport.pdf 30. International Society for the Study of Fatty Acids and Lipids (ISSFAL) Report on Dietary Intake of Essential Fatty Acids. Recommendations for Dietary Intake of Polyunsaturated Fatty Acids in Healthy Adults, June 2004. [Link] 31. Vannice G, Rasmussen H. Position of the Academy of Nutrition and Dietetics: dietary fatty acids for healthy adults. J Acad Nutr Diet. 2014;114:136-53. [PubMed] 32. Papanikolaou Y, Brooks J, Reider C and Fulgoni VL 3rd. U.S. adults are not meeting recommended levels for fish and omega-3 fatty acid intake: results of an analysis using observational data from NHANES 2003–2008. Nutr J. 2014;13:31. [PubMed] This Invited Opinion paper was written and prepared by the Global Organization for EPA and DHA (GOED), in collaboration with the Omega-3 Science Advisory Council (http://alwaysomega3s.com/see/science-advisory-council) Corresponding author: Elana Natker, MS, RD
Enlighten Nutrition, LLC
elana@enlightennutrition.com
Omega-3 Science Advisory Council
Cheryl Forberg, RD
Author, Nutritionist, Advisor
William (Bill) Harris, PhD
President, OmegaQuant
Professor, University of South Dakota
Daniel E Soffer, MD, FNLA
Clinical Associate Professor of Medicine
Division of General Internal Medicine at Perelman School of Medicine of the University of Pennsylvania
Marie Spano, MS, RD, CSCS, CSSD
Sports Dietitian, Journalist
Scientific Consultant
Dariush Mozaffarian, MD, PhD
Dean, Friedman School of Nutrition Science & Policy
Tufts University

